History of SAM
I am Dr Rhid Dowdle OBE – Retired. Formally Consultant Physician and Cardiologist, Royal Glamorgan Hospital, Cwm Taf Morgannwg University Health Board, Archivist of the Society for Acute Medicine

This document is written from my viewpoint and recollections, with significant additional input from:-
• Prof Derek Bell OBE – Group Chair of North Tees and Hartlepool NHS Foundation Trust and South Tees Hospitals NHS Foundation Trust. Formally Professor of Acute Medicine, Chelsea and Westminster Hospital NHS Foundation Trust and Imperial College London
• Prof Paul Jenkins – Retired. Formally Winthrop Professor of Acute Medicine, University of Western Australia, Perth, W.A. and Consultant Physician, Norfolk and Norwich University Hospital
• Dr Mike Jones - GIRFT National Clinical lead for Acute and General Medicine, Executive Medical Director Federation of Royal College of Physicians. Formally Consultant Acute Physician, County Durham and Darlington NHS Foundation Trust
• Dr Chris Roseveare - Consultant in acute and general medicine, Lymington New Forest Hospital, Southern Health NHS Foundation Trust, former editor of the Acute Medicine Journal from 2001 to 2017
We were all early enthusiasts in improving the care delivered to the acutely ill medical patient. Together we made up the medical membership of the first Executive Committee of the Society for Acute Medicine (SAM)
Prologue
Medicine has changed remarkably over the last 50 years. In the 1960s the vast majority of consultant physicians were involved in the care of acutely unwell medical patients, who were admitted to their wards on the acute medical intake. Consultant physicians specialising in single system disorders and not involved in acute patient care were in a clear minority, almost entirely confined to teaching hospitals and a small number of specialist hospitals.
Consultants at that time did indeed mainly consult. The majority of day to day care was provided by junior doctors in training – House Officers – supervised by more advanced trainees, Medical Registrars, who might provide cover for more than one hospital at any one time, even for the medical intake. Similarly, many consultants also had patients in more than one hospital.
It was unusual for consultant physicians to visit their wards every day, and some might only be present for the twice weekly consultant ward rounds. Contacting a consultant out-of-hours occurred rarely, even when on intake, and the medical registrar made the vast majority of decisions on day to day patient management.
It is therefore striking to consider in retrospect how little the medical consultants, the most experienced medical clinicians, were involved in direct care of acutely unwell patients. Indeed, several days might pass before an acutely admitted patient was seen by their consultant.
Problems in accommodating acute medical admissions were substantially less in the 1960’s, though there were always episodes when the system was stressed by pressure on beds and there was much variability from place to place. The numbers of hospital beds available were very different then. In 1974 the total number of NHS beds in England was around 400,000, by 1988 it had fallen to 299,400 and it fell a further 53% to 141,000 in 2020.
So much for the good old days!
Evolution
With the passage of time changes gradually occurred in acute medicine, usually as a response to changing circumstances and seldom due to considered planning. The first change was the inexorable increase in the number of medical admissions.
In Scotland, emergency admissions increased by 45% between 1981 and 1994 and there was a similar, 42% increase in England between 2006 and 2018. The reasons for this were, and still are, multifactorial, including increasing patient demand for medical care, which was often entirely justified, and increasing discomfiture in primary care in managing acutely unwell patients at home. This in turn may well have been influenced by awareness of the technical improvements in care available in hospital and the increasing publicity given to adverse events in patient care everywhere.
The increasing numbers of admissions produced a series of changes in hospital medical practice. In earlier days it had been usual for medical consultants to have all their patients on a single ward. This worked well for patient care as all those involved were familiar with that team’s policies. Members of both the nursing and medical teams became well acquainted personally and were well aware of each other’s strengths and weaknesses.
A consultant was therefore used to having designated medical beds, always available for their own patients. These beds would have been sufficient to accommodate the patients admitted during that consultant’s medical intake, with internal bed management by the relevant medical team ensuring vacant beds before expected periods of intake. As admission numbers increased, this formal bed holding became inadequate, and patients admitted on the acute intake spilled over into the beds designated to other consultants. Often this did not go down well with cries to the effect of “Get your patient out of my bed!” being not uncommon.
Once the inflow of patients had increased to the point where some admissions had to be accommodated on wards outside the admitting consultant’s domain, familiarity with both that team’s policies and staff declined, a situation obviously not conducive to best patient care. It also meant that the admitting team were now working in more than one location and time was spent in corridors that could have been better spent at patients’ bedsides. Additionally, the admitting team found themselves increasingly engaged in often difficult discussions regarding the placement of patients in beds allocated to other consultants.
If the overflow of acute admissions remained within the beds allocated to the Department of Medicine, there was some comfort in knowing that the ward staff would have current knowledge of the care of medical patients, and would be able to manage the new patients at least satisfactorily. However, when all available medical beds were occupied and acutely unwell medical patients had to be sent to non-medical wards the situation deteriorated significantly, both in terms of direct patient care and in the increasing discomfort of the ward staff faced with these patients, whose problems and needs were unfamiliar to them.
One solution to this situation would have been to have closed the hospital to further medical admissions, but this denial of service was considered unacceptable for a variety of reasons. Accordingly, a strategy was put in place which improved, but did not resolve, the problem. That strategy involved the creation of a new post - that of Hospital Bed Manager - whose main function was to arrange accommodation for the incoming acute medical admissions, and this role did at least free up otherwise unproductive medical time,
With the passage of time the ever-increasing presence of medical patients on surgical wards itself led to changes. In some hospitals some surgical beds were re-allocated to Medicine and were staffed by medically experienced staff. The development of Surgical Day Units allowed surgical activity to be maintained in the face of a falling number of surgical beds.
Whilst the creation of the post of Bed Manager took some of the heat out of the relationships between the medical and non-medical wards, the medical admitting teams were still walking the corridors to visit and revisit their increasing numbers of patients on “safari ward rounds”, wasting time that could be ill afforded. The rational solution to this problem was to admit all new admissions to a single clinical area, from which they might be discharged home after a short stay or transferred to the place where they would stay for the remainder of a more prolonged admission. Such a facility also improved the quality of patient care at the time of admission as now all patients could be assessed in an appropriate environment by appropriate staff.
By the early 1990s a number of such units, variously called Medical Assessment Units, Medical Admission Units (MAUs), Acute Medical Units (AMUs) or other similar terms had been established. Derek Bell recalls an overnight medical admissions facility being in place at the Royal Infirmary of Edinburgh (RIE) in 1986-7 and an AMU being created at the Central Middlesex Hospital in 1992. Paul Jenkins recalls that an AMU was opened at the Norfolk and Norwich University Hospital in 1993 and Mike Jones reported that Ward 15 at the Ninewells Hospital in Dundee had functioned essentially as an Acute Medical Unit since its inception in 1973
Some consultant physicians were now working mainly or entirely in these new units, managing the initial care of acutely ill medical patients referred to hospital. The terms Acute Care Consultant and Consultant Physician in Acute Medicine were being used to describe them. Paul Jenkins and Mike jones were appointed Acute Physicians in 1995 with Derek Bell acquiring a similar title in 1996 and Chris Roseveare in 1999. Such appointments were thought appropriate by the Scottish Intercollegiate Working Party on Acute Medical Admissions and the Future of General Medicine which commented in 1998 that “Large hospitals might consider appointing physicians in acute care medicine”.
However, not all AMUs were associated with the appointment of an Acute Physician and the majority of consultants working on the Acute Medical Unit remained General Physicians with other specialty interests, working as “Consultant of the day”. These Physicians both admitted and subsequently managed the patients of the acute medical intake and this was undertaken with varying degrees of enthusiasm.
As the volume of acute work increased, time available to work in a consultant’s associated specialty decreased and a tension developed between acute care and specialty care. In parallel to this, technological developments such as fibre-optic endoscopy and echocardiography made specialisation in District General Hospitals more practicable. This in turn led to a move by some consultants to favour their specialty over their more general work, and to endeavour to withdraw from involvement in the acute take, and particularly the continuing care of unselected medical patients, to concentrate on their chosen specialty alone. Thus there was a flight from general medicine in favour of specialisation.
Paradoxically, in some situations this encouraged the creation of new Acute Physician posts that could fill the gaps in acute care left by the departing specialists. Some of the job descriptions of these posts reflected that ambition alone. Not all of these new posts were filled at consultant level and some noteworthy early Acute Physicians started in their roles as Staff Doctors (Locally employed doctors) or Associate Specialists. Indeed, records from the RCPL of acute medicine post advertised between 1995 and 2000 indicate that the vast majority of such posts were advertised at Staff Doctor grade.
However, many General Physicians with specialist interests still remained committed to the challenging task of providing best care to the patients of the acute unselected intake, whilst maintaining their skills in their chosen specialty. This was my situation.
Our Acute Medical Unit, which comprised 16 beds and occupied half of an existing medical ward, opened in October of 1994. The immediate benefit of this strategy was that once again, all medical staff on the admitting team were working together at a single location, but there were also objections. Some of the medical wards were unhappy about no longer receiving acutely unwell medical patients from their first arrival in hospital. They missed the excitement of initial care. They also felt that having not been involved in this initial care, they never knew those patients as well as they had done previously. This discontinuity of patient care now demanded a patient handover process, something which had never been needed previously and which itself had to evolve.
On the other hand, there were unexpected benefits. Nursing and other staff who enjoyed working in an acute care area gravitated towards the Unit and rapidly acquired new skills, whilst staff who were less happy drifted away. A strong “esprit de corps” quickly developed on the Unit.
Since all acute medical admissions now entered the hospital’s administrative system through a single portal we now had good evidence of the actual numbers of our medical admissions as compared to the previous system which only counted apparent medical discharges. There was a significant difference!
Consultant involvement in the management of previously admitted patients also evolved over the years and consultant physicians in general became more frequent visitors to their wards at times other than ward rounds
When I became a consultant I soon discovered that if I spoke to the Medical Registrar on-call before going home on intake days, we could identify patients to whose care I could make a meaningful contribution. This reduced the number of phone calls I received at home and the number of times I needed to return to the hospital, but I must also protest that my rationale was not entirely selfish as I did have altruistic aspirations to deliver the best patient care. This conversation then became more formalised to a review of all newly admitted patients at their bedside and rapidly became accompanied by a similar ward round on the morning after a day on-intake. For me the Post-Take Ward Round sprung into being in 1980. This was not greeted with great joy by all of my consultant colleagues and those in some in other hospitals were said to have expressed concern at my mental wellbeing.
Some medical trainees were also attracted to acute care and Paul Jenkins established an acute medical registrar post, approved and supported by the East Anglian Deanery in 1997. We submitted an application for approval of an SHO post in Acute Care Medicine in our AMU in 1998.
Meanwhile, the Royal College of Physicians of London had become aware of the ever increasing number of consultant physicians working in Acute Medicine – an unrecognised specialty – as their sole clinical commitment, and also of the report of the Scottish Intercollegiate Working Party on Acute Medical Admissions and the Future of General Medicine. In early 1999 a working party of the then Federation of Royal Colleges of Physicians of the UK was convened, chaired by Prof Carol Black, then Clinical Vice President of the Royal College of Physicians of London (RCPL), to consider the status of these Acute Care Physicians. Later that year the Federation working party invited a number of clinicians who had been identified as active Acute Care Physicians or who had expressed an interest in Acute Care Medicine, to give evidence to the working party. This meeting took place at the Royal College of Physicians of London on 29th September 1999 and included 13 of the 22 Acute Care Physicians then in post.
The conclusions of the Federation working party, expressed in a report entitled ‘Acute Medicine: The Physician’s Role’, were somewhat at variance with the Scottish Colleges’ report. It not only failed to express enthusiasm for Acute Medicine as a specialty but its recommendations appeared in conflict in a number of ways. On the one hand, it was recognised that there was definitely a role for acute physicians, who should be involved in the emergency rota for acute medical intake, whilst, on the other hand, the report did not recommend either the appointment of physicians solely to provide acute care without links to a specialty, or a separate training programme for acute medicine. It did, however, recommend the further development of medical admission units. The term “Acute Medicine” and “Acute Care Physician” were used throughout the document – an indication that the Medical Royal Colleges did acknowledge the existence of both as concepts. These inconsistencies reflect the early stage of development of a proposal that was, in many ways, a radical departure from the traditional approach to management of acute general medical patients.
After the meeting on 29th September, a number of attendees adjourned to The Albany in Great Portland Street to consider events of the day.
After some conversation Derek Bell commented to the effect that, as we were all obviously interested in acute medicine, we should meet again. This suggestion could perhaps be considered to be the actual foundation of the Society for Acute Medicine.
Mike Jones however recalls that there was a Scottish meeting on Acute Medicine, held in Stirling in February of 1999, at which it was suggested that there should be a Society for Acute Medicine, but this suggestion however was not developed further.
The further meeting of this group of clinicians was facilitated by Prof David London, then Registrar of the RCPL, which took place at the College on November 26th, 1999. The involvement of the RCPL in setting up this meeting was encouraging, suggesting that the College was not entirely antagonistic to the development of Acute Medicine.
At that meeting an interest group was formed, the Acute Medical Group, within which two working parties were set up, one to address issues of terminology, structure of units and organisational structure and the other to address issues of quality and training.
I was tasked by the Group to explore the possibilities of liaison with the discipline of Accident and Emergency Medicine.
Membership of the Acute Medical Group comprised:-
• Derek Bell, Edinburgh
• Carole Connor, Edinburgh.
• Rhid Dowdle, East Glamorgan
• Peter Featherstone, Portsmouth
• Paul Jenkins, Norfolk and Norwich
• Mike Jones, Dundee
• Winnie Miller, Glasgow
• Graham Nimmo, Edinburgh
• Mairi Pollock, Edinburgh
• Tanzeem Raza, Bournemouth
• Chris Roseveare, Southampton
• Paul Schmidt, Portsmouth
The first formal meeting of the Acute Medical Group took place at the Royal College of Physicians of Edinburgh (RCPE) on 14th April 2000 with a clinical programme and a subsequent discussion of strategy.
This resulted in the foundation of the Society for Acute Medicine (UK), with the following elected officers and members co-opted to the executive committee.
• President Derek Bell
• Vice President Paul Jenkins
• Secretary Mike Jones
• Treasurer Chris Roseveare
• Nursing Representative Mairi Pollock Operational Manager, Acute Medicine, RIE
• Co-opted member Rhid Dowdle
• Administrator Audrey Deuchars Medical Assessment, RIE
I actively sought membership of the executive committee for two reasons, though neither was ever made explicit. Whilst the majority of the physicians making up the medical membership of the new executive committee were active Acute Physicians, the great majority of acute medical admissions throughout the UK were managed by physicians like myself, General Physicians with Specialist Interests, involved in the acute medical intake.
I felt it vital that the Society should not be perceived as being exclusive of such physicians, but should support those of us who remained committed to acute medicine.
Secondly I felt that for the Society to be representative of acute medicine in the UK, there should be representation from each nation with an independent health service.
Sadly at that time we had seen no interest from clinicians from Northern Ireland. For these reasons, I was delighted to have been co-opted onto the executive committee.
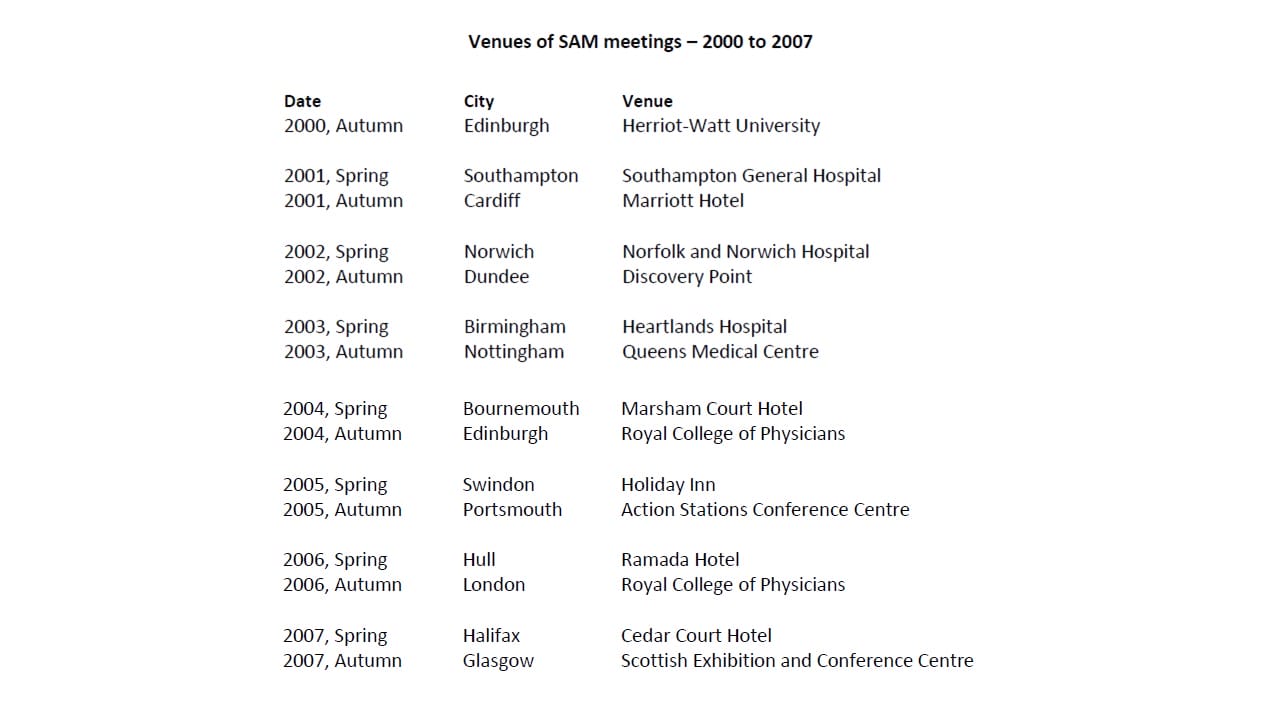
The first meeting of the new Society was held at Heriot Watt University, Edinburgh on October 5th 2000.
The Society for Acute Medicine
Following the Edinburgh meeting on 14th April 2000, the Society appointed an administrator, Audrey Deuchars - PA to Derek Bell at the Royal Infirmary of Edinburgh (RIE), set up a website - www.acutemedicine.org.uk and acquired an email address - admin@acutemedicine.org.uk.
Officers of the Society met in York in the summer of 2000 to agree a constitution for the Society and to decide its naming. Chris Roseveare recalls that “This was the subject of considerable debate, the final consensus being 'The Society for Acute Medicine (UK)”.
The first meeting of the new Society was held at Heriot Watt University, Edinburgh on October 5th 2000 and Derek Bell, as President included in the invitations to attend that were distributed, the following statement describing the aims and objectives of the Society. (Ref 11)
“The Society for Acute Medicine (UK) was founded in June 2000 by a group of like-minded clinicians who had met informally over the previous 12-18 months. Most of the group members had also given evidence to the Federation of Royal Colleges Report on ‘Acute Medicine: The Physicians Role’ published this year. The Society is intended to be a forum for clinicians and managers working in Acute Medicine with an emphasis on bringing together all the professions involved in the acute management of patients.
The Society intends to foster and develop links with other relevant societies and to promote education and training in acute medicine. The Society wishes to promote and develop clinical standards in conjunction with the Royal Colleges and to help determine national standards and audit priorities in this area. The next meeting of the group will be held in Edinburgh on 5 October 2000 in the Edinburgh International Conference Centre and meetings are planned for the following year in South Wales and Norfolk and Norwich.”
The invitation to attend also included a subscription form to join the Society, whose title rapidly became abbreviated to SAM(UK). Joining the Society attracted reduced attendance fees for future meetings and a reduced subscription to the Rila publication The CPD Journal of Internal Medicine, which was edited at that time by Paul Jenkins. This was adopted by the Society as its house journal in 2001 at which point it was provided free to all members paying a full subscription .
35 doctors and other clinical staff, 19 from Scotland, 13 from England, two from Northern Ireland and one from Wales, and from 15 different organisations attended this first meeting . The keynote speaker was Mr John Heyworth, President Elect of the British Association of Accident and Emergency Medicine.
The first meeting of the Executive Committee of SAM(UK) took place at this time and was attended by committee members Derek Bell - President, Mike Jones - Secretary, Chris Roseveare - Treasurer, Rhid Dowdle and Mairi Pollock. Members in attendance were Peter Featherstone, Paul Schmidt and Liz Myers. There were apologies from Paul Jenkins, Vice President, and from Simon Fletcher who had been appointed to liaise with the Intensive Care Society. Interestingly the value of scoring systems to assess patients’ clinical status was the topic of one of the workshops.
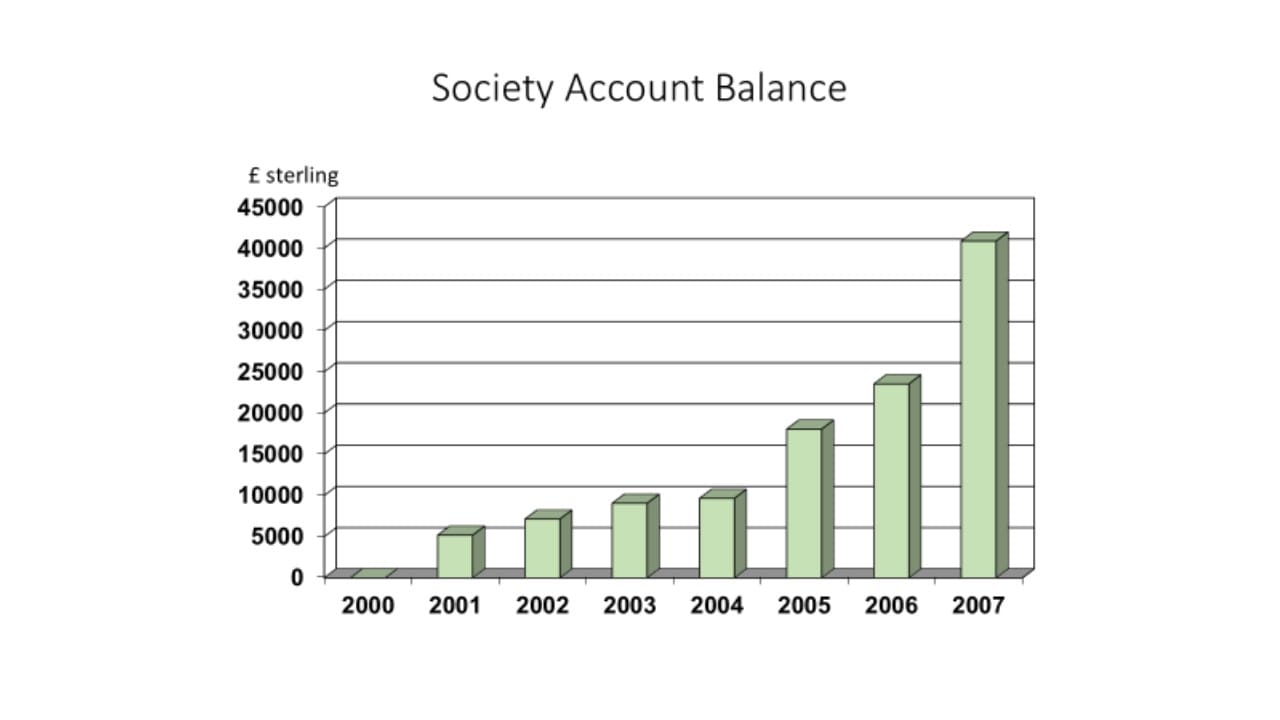
After this meeting the Society's financial reserves were in the order of £1500
It was decided in committee that SAM(UK) should hold meetings twice a year, in the spring and the autumn, scheduled on Friday afternoons and Saturday mornings. The next meetings planned were to be in Norwich on Friday 20th April, 2001 and Cardiff on Friday 5th October, 2001. Ultimately the Norwich meeting had to be re-scheduled and was replaced by a meeting in Southampton hosted by Chris Roseveare. The proposed cost for the forthcoming meetings would be £20 if membership were obtained at the same time and £10 for non-members.
The Southampton meeting took place on 20th April 2001 and included a parallel session on the development of nurses and members of the professions allied to medicine (PAMs) in Acute Medicine. A keynote speaker was Dr Gary Smith, ITU Consultant at the Queen Alexandra Hospital in Portsmouth, who spoke on multiprofessional training and the ALERT course.
The third meeting of SAM(UK) took place in Cardiff on the afternoon of Friday 5th and the morning of Saturday 6th, October, 2001. It was hosted by Rhid Dowdle.
The first Annual General Meeting (AGM) of the Society took place during this meeting. The Society by then had 89 members paying an annual subscription of £40 by standing order.
It was perceived that the executive committee needed to be augmented by further nurse representative, representation from each of the PAMs and from pharmacy. The constitution of the Society was amended to reflect this and earlier decisions.
The frequency of meetings was discussed again and it was agreed that the twice yearly frequency remained appropriate.
Future venues for the meetings were agreed to be Norwich in April 2002, Dundee in October 2002 and Nottingham in April 2003. It was also suggested that the 10th meeting of the society should be held in Europe.
By 2002 Derek Bell, in his letter to the membership as SAM(UK) President, commented that the term ‘Acute Medicine’ was beginning to creep into the medical vocabulary and the Society’s views were by then being sought by the Medical Royal Colleges and by Government on appropriate occasions.
The number of posts appointed in Acute Medicine throughout the country was still increasing. It was interesting to note that, whereas between 1995 and 2000 the vast majority of posts advertised in acute medicine in England and Wales, were at Staff Doctor grade, RCPL records show that in 2002 the situation had reversed with 23 appointments made at Consultant level and only 3 Staff Doctor appointments.
In my own hospital, we appointed our first formal Acute Physician in 2000 and he rapidly developed an interest in early patient discharge. With the help of a nursing sister and the use of a four bedded ward bay for follow-up outpatient visits, he was able to double the number of patients discharged within 24 hours of first being seen in the hospital. This was our first experience of ambulatory medical care, and it won us a Welsh National Healthcare Award.
Derek also reported that a number of regions in Scotland had been successful in developing specialty training programmes in Acute Medicine. Paul Jenkins had already established an acute medical registrar post, approved and supported by the East Anglian Deanery, in 1997.
This was initially a stand-alone post but subsequently became a rotational post within medicine, incorporating a 6 months placement in Intensive Care Medicine (ICM). Conversely registrars training in ICM in Norwich rotated through Acute Medicine for a six month period at the request of the local ICM trainers and with significant benefit to the Acute Medical service. Paul was passionate about trainees in Acute Medicine having significant exposure to Intensive Care Medicine.
At the start of 2002 Acute Medicine remained unrecognised as a speciality in its own right, however the RCPL then endorsed the development of the specialty of acute medicine and of an appropriate training programme in acute medicine, to be carried out under the auspices of General (Internal) Medicine training.
In early 2002 Mike Jones, as Secretary of SAM(UK), produced a curriculum for training in Acute Medicine with General (Internal) Medicine and by the autumn of that year new training numbers had been allocated for Specialist Registrar posts in General Internal Medicine, specifically designed to provide training for Acute Care Physicians in Wales.
In 2003, the Specialist Training Authority (STA) granted sub-specialty status for Acute Medicine. The support of Major General George Cowan OBE, Medical Director of the Joint Committee on Higher Medical Training (JCHMT) was crucial in this decision and this was acknowledged by the Society when Major General Cowan was made one of the first SAM Honorary Fellows in 2011.
A Higher Medical Training Curriculum for Sub-Specialty Training in Acute Medicine for General (Internal) Medicine NTN Holders was published by the JCHMT in July 2003. The curriculum stated that:-
“This document aims to outline the necessary skills that should be developed by an individual who aims to work in, and play a lead role in, a Medical Assessment or Medical Admissions unit (MAU). This differentiates the Acute Physician as laid out in this document from the physician who takes part in the acute take but is further qualified in another medical specialty and does not take a managerial role in the MAU”.
This is description is perhaps the first formal acknowledgement by the Medical Royal Colleges of the role of the Acute Physician.
![Ref17_-_JCHMT_Acute_Medicine_Curriculum_-_2003[1]-page-001 Ref17_-_JCHMT_Acute_Medicine_Curriculum_-_2003[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref17_-_JCHMT_Acute_Medicine_Curriculum_-_20031-page-001.jpg)
The Society’s Annual General Meeting for 2003 took place on 4th October at the Queens Medical Centre as part of the Society’s autumn meeting in Nottingham. Elections took place for new officers of the Society and the results were as follows:-
• President – Paul Jenkins,
• Vice President – Mike Jones,
• Secretary – Rhid Dowdle,
• Treasurer – Chris Roseveare,
• Ordinary Member – Phil Dyer (Birmingham Heartlands).
In view of the changing nature of the NHS it was proposed that there should be trainee representation from both North and South. Roger Duckitt and Steven Close joined the Executive Committee as trainee representatives. Mairi Pollock continued as Nursing Representative and was joined in this role by Liz Myers. Alastair Graham joined the Committee representing Allied Healthcare Professionals (AHPs), the successor organisation to PAMs, at the December Executive Committee meeting.
The Society now had 103 members, including 8 from nursing and the AHPs, and funds in the order of £7500.
Although the non-medical membership of the Society was small in comparison to the medical membership, the nursing representatives, Mairi Pollock, Liz Myers and Glynis Dack , put in an inordinate amount of work to develop the multidisciplinary aspect of the Society. The program for the Spring Meeting of the Society in Southampton in April of 2001 included the first session dedicated to nursing in Acute Medicine.
2004 was a memorable year for Acute Medicine, not only for the introduction of Modernising Medical Careers, but also for the publication in April 2004 of the RCPL report Acute medicine: making it work for patients.
This document contrasted significantly with Acute medicine: the physician’s role, its predecessor of 2000, in that the RCPL had now clearly recognised acute medicine as a new specialty and sought to define its clinical role and training requirements.
The working party that drew up the report was chaired by Alistair Douglas from the New Consultants Committee of the RCPL and included Derek Bell, representing SAM(UK), Mike Jones, representing the Royal College of Physicians of Edinburgh and Chris Subbe from the RCPL Trainees Committee. There was also input from Steven Close, Specialist Registrar in General Medicine from Aberdeen, Peter Featherstone from Portsmouth, Liz Lees, Consultant Nurse from Birmingham Heartlands Hospital, Tanzeem Raza from the Royal Bournemouth Hospital and Prof Bryan Williams from Leicester.
Many of the above maintained an interest in Acute Medicine, becoming members and officers of SAM(UK).
The report specifically made a number of recommendations including, amongst other things:-
• The following definition of ‘acute medicine’:
“Acute medicine is that part of general (internal) medicine concerned with the immediate and early specialist management of adult patients with a wide range of medical conditions who present in hospital as emergencies”.
• All trusts admitting acutely ill medical patients should have a dedicated area where they can be managed. Current terminology is confused, and we recommend the term ‘acute medicine unit’ (AMU)
• A consultant physician in acute medicine in every trust, who is given time to take the lead in the development and provision of acute medicine to ensure that this service, which is pivotal to the quality of care, is developed as a matter of urgency
• There should be at least three consultants with primary responsibility for acute medicine in every acute hospital… by the year 2008
• We recommend that an appropriately trained member of the clinical staff should assess according to clinical need, and certainly within four hours of arrival, all patients presenting to hospital as acute medical emergencies
• A doctor with appropriate skills in acute medicine should be present at all times in all units receiving acute medical emergencies. This would usually be a specialist registrar or equivalent …. who should have the MRCP(UK) Diploma or equivalent, and two years recent experience in managing patients presenting as acute medical emergencies.
• A consultant physician who has no other scheduled commitments should support this doctor.
• One hour should be allowed for assessment, documentation, investigation and result gathering, carrying out interventional procedures, treatment and prescription of therapy for each new patient presenting as an acute medical emergency
• 15 minutes for each new patient should be available on a consultant’s ‘post-take’ ward round
• Each new patient admitted should be reviewed by a consultant physician within 24 hours.
• Regional specialty advisers should be appointed jointly by the three Royal Colleges of Physicians of the UK and the Society for Acute Medicine to work with postgraduate deans on issues such as acute medicine training and its funding
• The three Royal Colleges of Physicians and the Society for Acute Medicine should work together with the Council of Heads of Medical Schools to establish a secure academic base for acute medicine.
Thus, not only was acute medicine now being formally recognised as a medical sub-speciality, but the Society for Acute Medicine (UK) was also being recognised as its representative body.
The Society by then had 185 members many of whom had become active in a variety of significant medical fora.
Paul Jenkins and Rhid Dowdle were members of the RCPL College Committee on Acute and General Internal Medicine, which had itself been renamed from the College Committee on General Internal Medicine as recommended in Acute medicine: making it work for patients.
Mike Jones was Secretary of the Speciality Advisory Committee (SAC) on General (Internal) Medicine of the Joint Committee for Higher Medical Training (JCHMT), of which Derek Bell and Rhid Dowdle were also members. Mike Jones also chaired the Joint Committee on Basic Medical Training (JCBMT), and reported much activity in relation to Acute Medicine in the Foundation years.
A working party had also been established with the RCPL on training in Acute Medicine for trainees in Emergency Medicine and Critical Care Medicine, chaired by Dr Alasdair Short, Consultant in Critical Care Medicine and immediate past Chairman of the Intercollegiate Board for Training in Intensive Care Medicine. Paul Jenkins and Mike Jones were members of this Working Party.
The following Acute Medicine Higher Training Programs were recognised in England and Wales:
East Anglia 4 posts at present with 4 more proposed
Wales 4 posts at present with 4 more proposed
Wessex 3 posts at present with 3 more proposed and 2 planned
North Trent 3 posts approved
Eastern 1 post approved
West Midlands 14 posts approved
South Trent 4 posts awaiting educational approval
South West Awaiting educational approval
The Society was increasingly being recognised as an authority on acute medical care and was asked to visit the Royal Free Hospital to advise on the provision of acute medical services there.
The Society recognised that a strong academic base was essential for the future development of acute medicine and the proposed establishment of a Chair in Acute Medicine at the Chelsea and Westminster Hospital by Prof Sir Leszek Borysiewicz, then Deputy Rector of Imperial College London, was welcomed.
The Society produced its first formal documents on clinical standards - Recommendations for Nurse Staffing on Acute Medicine / Medical Assessment Units and Guidelines for Physiotherapy in Medical Assessment Units
In 2005 concerns arose in the SAM(UK) Executive Committee about the potential financial liabilities of individual officers and the need for indemnity insurance. The case for the Society acquiring charitable status was discussed and it was decided to take this to the next AGM
The Society by then had more than 250 members and it was confirmed that 83 NTNs had been issued for training in Acute and General (Internal) Medicine in England and Wales. The first CCT holders were expected in 2007.
The Society’s house journal had evolved over the preceding five years. Chris Roseveare took over the role of editor in 2002, at which point the journal was renamed the CPD Journal of Acute Medicine and subsequently Acute Medicine in 2005
The prospective SAM logo was discussed with the membership at the meeting in Swindon and accepted at the subsequent meeting in Portsmouth.

The autumn meeting of the Society in 2006 was planned to be held in the RCPL on September 21st & 22nd, and presented a financial challenge. The deposit for the use of the 300 seat Wolfson Theatre alone being £6000, with costs to the Society of £100 per day per delegate!
The Society had now been registered with the Advisory Committee on Clinical Excellence Awards (ACCEA) and was able to support members’ nominations for awards.
The Department of Inland Revenue also agreed that the cost of annual subscriptions to SAM(UK) could be allowed as an income tax deduction!
Elections of officers of the Society had resulted in a new Executive Committee which, in March 2006, comprised:-
• President - Mike Jones
• Vice President and President-elect - Rhid Dowdle
• Secretary - Phil Dyer
• Treasurer - ` Chris Roseveare
• Ordinary Member - Alistair Douglas
• Critical Care Liaison - Simon Fletcher
• Nursing Representative - Liz Myers
• Nursing Representative - Glynis Dack
• Trainee Representative - Roger Duckitt
• Trainee Representative - Hannah Skene
• AMP Representative - Alastair Graham
Derek Bell was appointed Professor of Acute Medicine at the Chelsea and Westminster Hospital and was asked to act as Academic Representative for the Society.
As the Society’s meetings were becoming more complicated it was decided that there should be a sub-committee of the Executive Committee tasked with organising future meetings, the format of which had now been defined in some detail. This subcommittee would comprise:-
• Chair - Immediate Past SAM(UK) President
• Expert organiser – Chris Roseveare
• Current SAM(UK) President
• A Trainee representative
• A Nurse representative
• The AHP representative
• The Local Organiser
Concerns about the financial probity of the society had led to discussions within the Executive Committee on the Society acquiring charitable status. This was thought an appropriate development and Mike Jones agreed to modify the constitution for the society to bring it in line with the constitution required for a charitable organisation.
Derek Bell and Mike Jones suggested that the Society should structure its forthcoming meeting in Glasgow as an international meeting. Derek was in contact with Christine Lawson from Eventage (Eventage.co.uk), an organisation that regularly managed such meetings, and felt that they could promote the Society and make a success of a bigger meeting than any that SAM(UK) had held previously. The venue suggested was the Scottish Exhibition and Conference Centre (SECC) and the number of attendees for this meeting to break even was around 420. A great deal of discussion took place in the Executive Committee on the pros and cons of this venture, in particular regarding the financial risk. Previous meetings had mainly been held in hotels where costs of hundreds of pounds were usual. The Society’s autumn meeting of 2006 took place in the RCPL and incurred costs of thousands of pounds including a deposit of £6000. However, expected costs of the proposed Glasgow meeting, including the cost of the venue and fees to Eventage, would be tens of thousands of pounds and would far exceed the Society’s financial reserves. An additional risk factor for this meeting was the threat of an H5N1 bird flu outbreak spreading to the UK from Europe and causing cancellation of the study leave of potential attendees. It was not found to be possible to insure against an inadequate number of attendees. After much debate seven members of the Executive Committee agreed to accept joint liability for any financial shortfall resulting from the meeting. My recollection of my wife’s expression when I told her what I had agreed to was indeed memorable!
The first International Meeting of SAM(UK) opened at the SECC on Monday 1st October 2007 (Ref 22). Subsequently Christine Lawson, as conference organiser, reported excellent feedback from the conference evaluation and the conference accounts showed a small profit, which was a good result considering that the aim was to break even. There was much relief in certain quarters!
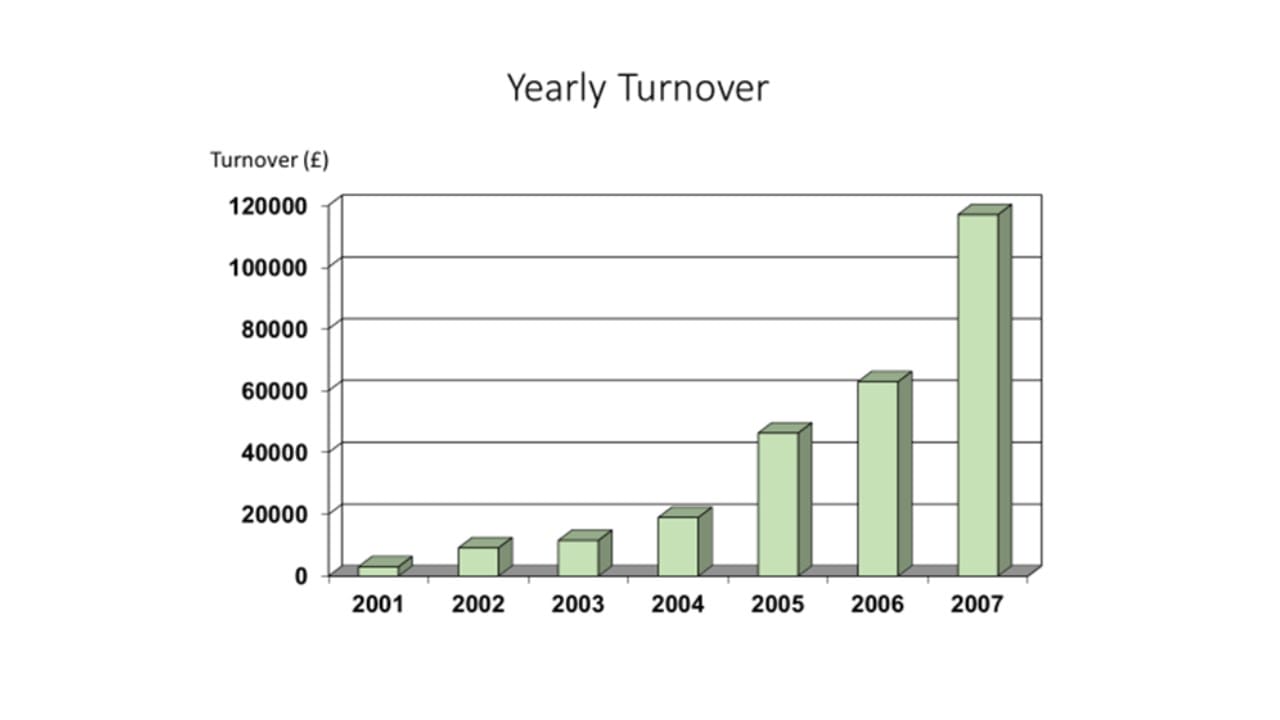
The Society’s finances had by now become substantial and the turnover for 2007 was over £100,000 with an end of year balance of £40,000.
The Executive Committee of SAM had decided soon after the Society’s formation that the venues for the two meetings each year should be widely distributed over the UK, but also needed to be readily accessible and to have attracted local members prepared to organise the meetings. The table below shows the venues for SAM meetings for the first seven years of its existence
Venues of SAM meetings – 2000 to 2007

![The_continuing_rise_in_emergency_admissions_-_The_BMJ[1]-images-0 The_continuing_rise_in_emergency_admissions_-_The_BMJ[1]-images-0](https://www.acutemedicine.org.uk/wp-content/uploads/The_continuing_rise_in_emergency_admissions_-_The_BMJ1-images-0.jpg)
![Emergency_hospital_admissions_in_England[1]-page-001 Emergency_hospital_admissions_in_England[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Emergency_hospital_admissions_in_England1-page-001.jpg)
![Ref6_-_Acute_Medical_Admissions_and_the_Future_of_General_Medicine_-_Scotland[1]-page-001 Ref6_-_Acute_Medical_Admissions_and_the_Future_of_General_Medicine_-_Scotland[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref6_-_Acute_Medical_Admissions_and_the_Future_of_General_Medicine_-_Scotland1-page-001.jpg)
![Ref7_-_Acute_Medicine_-_the_physician s_role[1]-page-001 Ref7_-_Acute_Medicine_-_the_physician s_role[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref7_-_Acute_Medicine_-_the_physician-s_role1-page-001.jpg)
![Ref8_-_Scottish_Acute_Medicine_Meeting_-_Feb_1999[1]-page-001 Ref8_-_Scottish_Acute_Medicine_Meeting_-_Feb_1999[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref8_-_Scottish_Acute_Medicine_Meeting_-_Feb_19991-page-001.jpg)
![Ref9_-_Minutes_of_Acute_Medicine_meeting_-_RCPL_-_26_Nov_1999[1]-page-001 Ref9_-_Minutes_of_Acute_Medicine_meeting_-_RCPL_-_26_Nov_1999[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref9_-_Minutes_of_Acute_Medicine_meeting_-_RCPL_-_26_Nov_19991-page-001.jpg)
![Ref10_-_Acute_Medicine_Group_Meeting_-_14_April_2000[1]-page-001 Ref10_-_Acute_Medicine_Group_Meeting_-_14_April_2000[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref10_-_Acute_Medicine_Group_Meeting_-_14_April_20001-page-001.jpg)
![Ref11_-_Invitation_to_Attend_SAM_Meeting_at_Heriot_Watt_University_on_5th[1]-page-001 Ref11_-_Invitation_to_Attend_SAM_Meeting_at_Heriot_Watt_University_on_5th[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref11_-_Invitation_to_Attend_SAM_Meeting_at_Heriot_Watt_University_on_5th1-page-001.jpg)
![Ref12_-_Minutes_of_first_SAM_Committee_Meeting_-_Edinburgh_Oct_2000[1]-page-001 Ref12_-_Minutes_of_first_SAM_Committee_Meeting_-_Edinburgh_Oct_2000[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref12_-_Minutes_of_first_SAM_Committee_Meeting_-_Edinburgh_Oct_20001-page-001.jpg)
![Ref13_-_Amended_Constitution_of_the_Society_for_Acute_Medicine_-_Oct_2001[1]-page-001 Ref13_-_Amended_Constitution_of_the_Society_for_Acute_Medicine_-_Oct_2001[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref13_-_Amended_Constitution_of_the_Society_for_Acute_Medicine_-_Oct_20011-page-001.jpg)
![Ref14_-_President s_Letter_2002[1]-page-001 Ref14_-_President s_Letter_2002[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref14_-_President-s_Letter_20021-page-001.jpg)
![Ref15_-_Acute_Medicine_-_Curriculum_for_Consideration_by_JCHMT[1]-page-001 Ref15_-_Acute_Medicine_-_Curriculum_for_Consideration_by_JCHMT[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref15_-_Acute_Medicine_-_Curriculum_for_Consideration_by_JCHMT1-page-001.jpg)
![Ref16_-_Acute_Medicine_-_the_application_was_approved_as_a_sub-specialty_by_STA[1]-page-001 Ref16_-_Acute_Medicine_-_the_application_was_approved_as_a_sub-specialty_by_STA[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref16_-_Acute_Medicine_-_the_application_was_approved_as_a_sub-specialty_by_STA1-page-001.jpg)
![Ref18_-_SAM_AGM_Minutes_-_October_2003[1]-page-001 Ref18_-_SAM_AGM_Minutes_-_October_2003[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref18_-_SAM_AGM_Minutes_-_October_20031-page-001.jpg)
![Ref19_-_Acute_medicine_-_making_it_work_for_patients_-_report[1]-page-001 Ref19_-_Acute_medicine_-_making_it_work_for_patients_-_report[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref19_-_Acute_medicine_-_making_it_work_for_patients_-_report1-page-001.jpg)
![Ref20_-_Acute_medicine_-_making_it_work_for_patients_-_Carol_Black[1]-page-001 Ref20_-_Acute_medicine_-_making_it_work_for_patients_-_Carol_Black[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref20_-_Acute_medicine_-_making_it_work_for_patients_-_Carol_Black1-page-001.jpg)
![Ref21_-_Draft_MAU_nurse_staffing_recomendations_-_2003[1]-page-001 Ref21_-_Draft_MAU_nurse_staffing_recomendations_-_2003[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref21_-_Draft_MAU_nurse_staffing_recomendations_-_20031-page-001.jpg)
![Ref22_-_SAM_Glasgow_2007_-_Final_Delegate_Guide[1]-page-001 Ref22_-_SAM_Glasgow_2007_-_Final_Delegate_Guide[1]-page-001](https://www.acutemedicine.org.uk/wp-content/uploads/Ref22_-_SAM_Glasgow_2007_-_Final_Delegate_Guide1-page-001.jpg)