Training Hub
Tips to get the most out of your training
1. Get your 20%
The standard is 1 day a week and this should be written into your departmental timetable. Taking a whole day is usually easier than 2 half days as you otherwise end up getting caught up in clinical work. It also means you can travel to other sites if needed (e.g. for POCUS days). If it works better for your specialist skill training to take your 20% in another format such as blocking it together as a week or more then that is something to consider early and arrange it with your supervisor and department.

2. Get an AIM and specialty skill supervisor
The gold standard is that your educational supervisor should be an acute medical consultant even if you are on specialty placements (plus a clinical supervisor would be in that specialty). This isn’t always the case but it is worth asking for as they understand your educational requirements and can support your progression. It is also recommended to have a supervisor for your specialist skill. Many of the specialist skills now require you to evidence certain levels of knowledge and have WPBAs in this area which your specialty skill supervisor will be able to help with. As a trainees choice of specialist skill is up to them it is expected that you source your own supervisor/mentor.
3. Regular Supervised PTWR
It is easy as an acute medicine registrar to take on a lot of the non-consultant work load such as ‘post-post-take’ ward rounds. Whilst these are part of the job, supervised post-take ward rounds offer a better training experience. Agree with a consultant at the start of the shift to reverse roles for the post-take ward round. This is a really good way to gain confidence in being the senior decision maker and work towards a consultant role. Try and do this regularly (weekly if you can) as a nice way to work more closely with your consultants, gain constructive feedback and complete WPBAs.

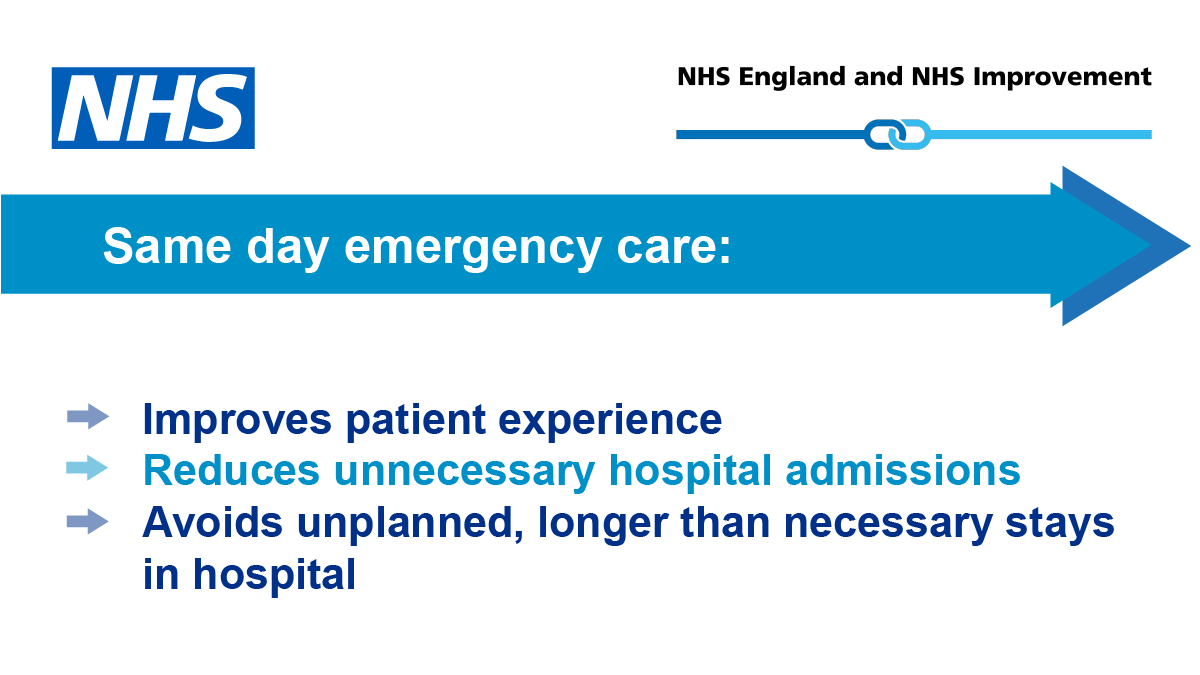
4. Dedicated SDEC / ambulatory care sessions
Whilst it is no longer an ARCP requirement to see a specific number of ambulatory care patients (hurrah!) it is still essential that you gain confidence in this core area of acute medicine. Depending on your needs and prior experience you may agree with your supervisor to have a regular day or more in ambulatory care. There are usually opportunities to take a leadership role (with consultant support available if needed) or work more closely with community settings by holding the referrals phone etc.
5. Network with other trainees
(Training days, WhatsApp groups locally and nationally, SAM events)
Training in acute medicine is great but we are all aware of the specific pressures we face and the harder elements of training such and frequent rotations, commuting, on call burden. Local trainee WhatsApp groups are usually really supportive for questions, venting, support and general chat. Seeing other trainees and colleagues face to face outside the ward also makes a huge difference. Try to get to these events both for support but also networking, keeping up-to-date and inspiration. Our field of medicine has lots of exciting things happening and this is the best way to hear about it.


6. Take advantage of opportunities
(Trainee rep, teaching, developing pathways, leadership fellowships, clinical fellowships, committees and national projects, takeAIM)
Acute Medicine training is wonderfully flexible and you only need to ask a few trainees to find out they have done all sorts of interesting things during this time. Whether it is a hospital-based opportunity or a national role you are interested in, it can usually be worked into your job plan. Make sure to liaise with your supervisor and TPD if you are going to need ring fenced time. All these opportunities are not only great for the CV but they can help to direct your interests and career possibilities.